INTESTINAL PROTOZOA
INTESTINAL PROTOZOA
INTESTINAL PROTOZOA
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
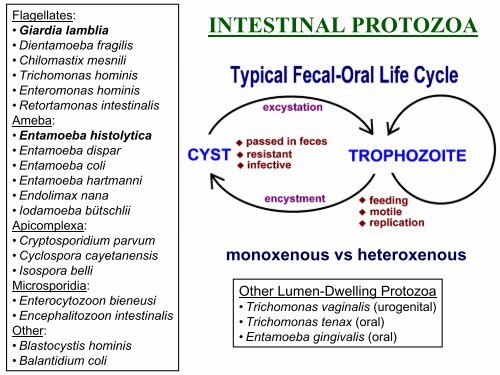
Flagellates:<br />
• Giardia lamblia<br />
• Dientamoeba fragilis<br />
• Chilomastix mesnili<br />
• Trichomonas hominis<br />
• Enteromonas hominis<br />
• Retortamonas intestinalis<br />
Ameba:<br />
• Entamoeba histolytica<br />
• Entamoeba dispar<br />
• Entamoeba coli<br />
• Entamoeba hartmanni<br />
• Endolimax nana<br />
• Iodamoeba bütschlii<br />
Apicomplexa:<br />
• Cryptosporidium parvum<br />
• Cyclospora cayetanensis<br />
• Isospora belli<br />
Microsporidia:<br />
• Enterocytozoon bieneusi<br />
• Encephalitozoon intestinalis<br />
Other:<br />
• Blastocystis hominis<br />
• Balantidium coli<br />
<strong>INTESTINAL</strong> <strong>PROTOZOA</strong><br />
monoxenous vs heteroxenous<br />
Other Lumen-Dwelling Protozoa<br />
• Trichomonas vaginalis (urogenital)<br />
• Trichomonas tenax (oral)<br />
• Entamoeba gingivalis (oral)
Taxonomy<br />
• one human species, aka:<br />
• G. duodenalis<br />
• G. intestinalis<br />
• morphologically similar<br />
forms in other mammals<br />
Giardia lamblia<br />
• worldwide distribution<br />
• higher prevalence in tropical or<br />
developing countries (20%)<br />
• 1-6% in temperate countries<br />
• most common protozoa in stools<br />
• ~200 million cases/yr<br />
• giardiasis<br />
• often asymptomatic<br />
• acute or chronic diarrhea<br />
Historical Notes<br />
1681 van Leeuwenhoek<br />
observed<br />
1859 Lambl documented<br />
1920’s clinical symptoms,<br />
but controversial<br />
1954 Rendtorff fulfilled<br />
Koch’s postulate
Fecal-Oral Transmission Factors<br />
•poor personal hygiene<br />
• children (eg, day care centers)<br />
• food handlers<br />
•developing countries<br />
• poor sanitation<br />
• endemic<br />
• travelers diarrhea<br />
•water-borne epidemics<br />
•male homosexuality<br />
• oral-anal contact<br />
•zoonosis?<br />
• Entamoeba =no<br />
• Cryptosporidium =yes<br />
• Giardia =controversial<br />
Is giardiasis a zoonosis?<br />
• no definitive documentation<br />
• transmission between<br />
humans and dogs rare<br />
(J.Parasit. 83:44, 1997)<br />
• person-to-person transmission<br />
is most prevalent
Giardia Life Cycle<br />
CYST<br />
TROPHOZOITE<br />
Infective stage<br />
passed in feces<br />
Replicative stage<br />
inhabiting sm. intestine
In Vitro Culture of Giardia<br />
Excystation<br />
• brief exposure to acidic pH (~2)<br />
• flagellar activity within 5-10 min<br />
after return to neutral pH<br />
• breakdown of cyst wall<br />
(proteases)<br />
• trophozoite emerges from cyst<br />
• cytokinesis within 30 min<br />
Encystation<br />
• exposure to pH 7, no bile<br />
• exposure to pH 7.8, high<br />
bile<br />
• cyst wall secretion<br />
(appearance of vesicles)<br />
• loss of disk and flagella<br />
• nuclear division
microtubules +<br />
microribbons<br />
lateral crest<br />
Adhesive Disk<br />
Components<br />
•microtubules<br />
• tubulin<br />
•microribbons<br />
• giardins<br />
•lateral crest<br />
• actin-myosin<br />
Attachment Mechanisms?<br />
• contractile ring<br />
• hydrodynamic force<br />
• receptor mediated
Clinical Features and Symptoms<br />
Range of Outcomes<br />
• asymptomatic/latent<br />
• acute short-lasting diarrhea<br />
• chronic/nutritional disorders<br />
Acute Symptoms<br />
Subacute/Chronic<br />
• recurrent diarrheal<br />
episodes<br />
• cramps uncommon<br />
• sulfuric belching, anorexia,<br />
nausea frequent<br />
• can lead to weight loss<br />
and failure to thrive<br />
• 1-2 week incubation<br />
• sudden explosive, watery diarrhea<br />
• bulky, frothy, greasy, foul-smelling stools<br />
• no blood or mucus<br />
• upper gastro-intestinal uneasiness, bloating, flatulence,<br />
belching, cramps, nausea, vomiting, anorexia<br />
• usually clears spontaneously (undiagnosed), but can<br />
persist or become chronic
Pathogenesis<br />
• epithelial damage<br />
• villus blunting<br />
• crypt cell hypertrophy<br />
• cellular infiltration<br />
• malabsorption<br />
• enzyme deficiencies<br />
• lactase (lactose<br />
intolerance)<br />
Possible Mechanisms<br />
• mechanical irritation<br />
• obstruction of absorption
Diagnosis<br />
• suspect: acute or chronic<br />
symptoms<br />
• confirmed: detection of<br />
parasite in feces or duodenal<br />
aspirate or biopsy<br />
• parasite easy to identify<br />
• parasite can be difficult to<br />
detect<br />
• inconsistent excretion in<br />
feces<br />
• patchy loci of infection<br />
Parasite Detection<br />
Stools<br />
• 3 non-consecutive<br />
days<br />
• wet mounts or stained<br />
• IFA, copro-antigens<br />
Aspirate or Biopsy<br />
• Enterotest (or string<br />
test)
Treatment<br />
Drug of Choice<br />
• metronidazole (Flagyl)<br />
• 750 mg/tid/5d<br />
• >90% cure rate<br />
Alternatives<br />
• tinidazole (single dose)<br />
• paromomycin (pregnancy)<br />
• quinicrine<br />
• furazolidone<br />
Prognosis is good<br />
with no sequelae<br />
Control<br />
• avoid fecal-oral transmission<br />
• improve personal hygiene<br />
• especially institutions<br />
• treat asymptomatic carriers<br />
• eg, family members<br />
• health education<br />
• hand-washing<br />
• sanitation<br />
• food handling<br />
• protect water supply<br />
• treat water if questionable<br />
• boiling<br />
• iodine<br />
• not chlorine
TRICHOMONADS<br />
• 3-5 anterior flagella<br />
• one undulating membrane<br />
• axostyle<br />
• hydrogensome (EM)<br />
Human Trichomonas Species<br />
T. tenax oral cavity<br />
T. hominis* intestine<br />
T. vaginalis uro-genital<br />
*aka: Pentatrichomonas
Trichomonas vaginalis<br />
• trophozoite stage transmitted<br />
during sexual intercourse<br />
• non-sexual contact possible<br />
• common STD<br />
• co-infection w/other STDs<br />
• more prevalent in at risk groups<br />
• associated with epithelium of<br />
uro-genital tract<br />
• females: vagina<br />
• males: urethra, prostate, epididymis<br />
• both sexes equally susceptible<br />
• symptoms more common in<br />
females<br />
sexual<br />
intercourse
In females:<br />
In males:<br />
Trichomoniasis<br />
• ranges from asymptomatic, to mild or<br />
moderate irritation, to extreme vaginitis<br />
• 50-75% abnormal discharge (frothy, yellowish or<br />
greenish)<br />
• 25-50% pruritis<br />
• 50% painful coitus<br />
• onset or exacerbation often associated with<br />
menstruation or pregnancy<br />
• vaginal erythema, ‘strawberry cervix’ (~2%)<br />
• 50-90% are asymptomatic<br />
• mild dysuria or pruritus<br />
• minor urethral discharge
DIAGNOSIS<br />
• demonstration of parasite<br />
• direct observation or in vitro<br />
culture<br />
• vaginal discharge<br />
• urine sediment<br />
• prostatic secretion<br />
TREATMENT<br />
• metronidazole (Flagyl)<br />
• 250 mg (3/d) for 5-7 days<br />
• single 2 g dose<br />
• simultaneous treatment of partner!<br />
(85-90% cure rate)<br />
PREVENTION<br />
• limit # of sexual<br />
partners<br />
• condoms
Key Features of Cysts<br />
• oval shape<br />
• 11-14 x 6-10 µm<br />
• distinct cell wall set apart<br />
from cytoplasm<br />
• 4 nuclei at anterior end<br />
• large karyosome, no<br />
peripheral chromatin<br />
• fibrils (axonemes) evident<br />
• median bodies
Key Features of Trophozoites<br />
• pear shape<br />
• 12-15 x 5-10 x 2-4 µm<br />
• 2 nuclei<br />
• large karyosome, no<br />
peripheral chromatin<br />
• fibrils (axonemes) evident<br />
• bilateral symmetry<br />
• pair of median bodies<br />
• adhesive disk (not always<br />
evident)<br />
• 4 pair flagella<br />
• motility likened to falling<br />
leaf
Other Flagellates Found<br />
in Human Feces<br />
• Dientamoeba fragilis<br />
• no flagella (discuss with amebas)<br />
• Pentatrichomonas hominis<br />
• formerly called Trichomonas hominis<br />
• Chilomastix mesnili<br />
• Enteromonas hominis<br />
• Retortamonas intestinalis
Non-Pathogenic Intestinal Flagellates<br />
Trichomonas hominis<br />
• 7-15 mm trophozoite<br />
• no cyst<br />
• single nucleus<br />
• axostyle<br />
• 4 free flagella +<br />
undulating membrane<br />
• costa
Non-Pathogenic<br />
Intestinal Flagellates<br />
Chilomastix mesnili<br />
• 10-20 mm trophozoite<br />
• 6-20 mm cyst<br />
• single nucleus<br />
• 4 flagella<br />
• cytostome
T. hominis<br />
Chilomastix mesnili